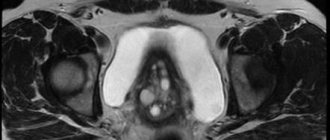
The uterus is an unpaired reproductive organ in women, which is located in the middle third of the pelvic cavity. In front of the uterus is the bladder, and behind are the middle and lower ampullae of the rectum, as can be seen in the photo. The weight of the uterus in women of reproductive age ranges from 40 to 70 g, in women who have given birth - up to 90 g.
The length of the organ is 4-8 cm, and the width is 5 cm. In women giving birth, the size of the uterus changes due to hypertrophy of the muscular wall. The uterus consists of three sections (from top to bottom): fundus, body and cervix. The wall of each section is represented by three layers: endometrium, myometrium, perimeter.
General structure of the uterus
This internal muscular organ of the reproductive system has a pear-shaped shape that is flattened in front and behind. In the upper part of the uterus on the sides there are branches - fallopian tubes, which pass into the ovaries. The rectum is located behind, and the bladder is located in front.
The anatomy of the uterus is as follows. The muscular organ consists of several parts:
- The fundus is the upper part, which has a convex shape and is located above the line of origin of the fallopian tubes.
- A body into which the bottom smoothly passes. It has a cone-shaped appearance. It narrows downwards and forms an isthmus. This is the cavity leading to the cervix.
- Cervix - consists of the isthmus, cervical canal and vaginal part.
The size and weight of the uterus vary from person to person. The average weight for girls and nulliparous women reaches 40–50 g.
The anatomy of the cervix, which is a barrier between the internal cavity and the external environment, is designed so that it protrudes into the anterior part of the vaginal vault. At the same time, its posterior arch remains deep, and the anterior arch, on the contrary.
Features of the development of cervical diseases, symptoms
At the moment, the problem of cervical disease still remains relevant. Such diseases are more common among girls of reproductive age.
Pathological changes often occur on the vaginal surface of the cervix, in the “transition zone” of one epithelium to another. When the localization of this zone changes, background diseases arise: ectopia (pseudo-erosion), ectropion, leukoplakia, erythroplakia, polyps and, as a consequence, malignant neoplasms of the cervix.
Ectopic cervix
Ectopia (pseudo-erosion) is a disease of the cervix, characterized by the emergence of columnar epithelium on the vaginal surface of the cervix. Women with irregular menstrual cycles are predisposed to developing this disease.
The clinical picture is somewhat blurred. Such women may complain of the release of blood clots after intercourse and the pain of the process of intercourse itself. The disease can be recognized during a medical examination of the cervix in the mirror: the surface of the organ will not be pale pink, but a bright red hue.
Cervical ectropion
Ectropion is an eversion of the mucous membrane of the cervical canal into the vagina, with the formation of scars and ectopia on the cervix. This disease occurs as a result of unsuccessful diagnostic or surgical intervention on the uterus, as well as after labor or abortion.
The clinical picture is calm - women do not complain or note minor discomfort in the lower abdomen of a pulling nature. There is no bleeding.
Leukoplakia of the cervix
Leukoplakia is a disease associated with the appearance of keratinized areas on non-keratinized epithelium. Leukoplakia can be simple or proliferative. The proliferative form is a precancerous condition and when biological material is taken from this area (biopsy), atypical cells are found.
There are no clear symptoms of the disease. This disease usually develops in women with disrupted hormonal levels or immune systems. With cervical trauma, the likelihood of developing the disease is high.
Erythroplakia of the cervix
With erythroplakia, the cervix is affected locally, closer to the external os. The pathogenesis of the disease is the thinning of the stratified squamous epithelium and, as a result, tissue atrophy. The etiology of erythroplakia has not yet been studied. The photo clearly shows red spots in the ectocervix area.
Cervical polyps
Polyps are growths of various sizes on the mucous membrane of the cervical canal. According to their structure, polyps are epidermal and glandular. When examined in a speculum, the polyps are oblong and leaf-shaped. It is possible to diagnose and differentiate such polyps only with an ultrasound examination of the pelvic area.
Cervical endometriosis
Cervical endometriosis is a disease in which tissue similar in structure to the endometrium is located on the vaginal surface of the cervix. Normally, such tissue should be located in the uterine cavity.
The main reasons for the development of this disease:
- cervical injuries due to violence, childbirth or abortion, as well as medical interventions;
- genetic predisposition;
- hormonal disbalance.
Patients with cervical endometriosis usually do not present characteristic complaints. There is discomfort during sexual intercourse, bleeding after intercourse, as well as before and after menstruation.
Cervical cancer
Cervical cancer (CC) is a malignant neoplasm of the cervix. The location and form of cancer is varied. The main component of the disease is atypical cells that can divide uncontrollably and replace healthy cells. In 90% of all cases, the cause of cervical cancer is the human papillomavirus. The main route of transmission of the pathogen is sexual intercourse.
Factors that increase the risk of developing the disease:
- early onset of sexual activity (before 17 years of age);
- failure to comply with hand and body hygiene rules;
- the presence of precancerous conditions (proliferative leukoplakia, polyps);
- frequent change of sexual partners;
- bad habits;
- infection with the papilloma virus in another way (during medical interventions, transmission from mother to fetus).
Clinically, it is difficult to suspect cancer in the early stages. Patients do not complain, there may be no discharge.
With progression, when the malignant disease moves to the next stage and grows, bleeding and nagging pain may appear in the lower abdomen. CC can be suspected only by performing a biopsy of the affected tissue for the presence of atypical cells.
Where is the uterus?
The organ is located in the pelvis between the rectum and bladder. The uterus is a very mobile organ, which also has individual characteristics and shape pathologies. Its location is significantly influenced by the condition and size of neighboring organs. The normal anatomy of the uterus in terms of the place it occupies in the small pelvis is such that its longitudinal axis should be oriented along the axis of the pelvis. Its bottom is tilted forward. When the bladder is full, it moves back a little, and when emptying, it returns to its original position.
The peritoneum covers most of the uterus except the lower part of the cervix, forming a deep pouch. It extends from the bottom, goes to the front and reaches the neck. The posterior part reaches the wall of the vagina and then passes to the anterior wall of the rectum. This place is called the pouch of Douglas (recess).
Diagnosis of cervical diseases
The doctor may suspect some pathological conditions of the cervix during a gynecological examination (examination of the organ in the speculum). Such a diagnosis is informative only for diseases affecting the vaginal part of the cervix. The cervical canal is inaccessible at this stage.
Taking smears from the cervical canal with a special brush for bacterial culture is a painful but informative procedure.
To clarify the diagnosis, the gynecologist resorts to the Schiller test - the use of iodine to identify pathological areas. Healthy cervical cells will intensively absorb iodine, turning brown, and areas of the lesion where there are no such cells will become pale.
Ultrasound diagnostics of the pelvic organs is informative in severe conditions - cancer, endometriosis. Such an examination is carried out in order to exclude damage to the body and fundus of the uterus, as well as the spread of the disease to neighboring organs.
Colposcopy makes it possible to evaluate the morphology of cells, thanks to the magnifying ability of the colposcope. Taking a biopsy is an extreme diagnostic measure, which the gynecologist resorts to if previous methods are not informative.
The purpose of a biopsy is to take tissue at the border of a healthy zone and a lesion for cytological examination in order to determine the presence of cancer cells in the biomaterial. Sometimes doctors use CT scan data to detect metastases (distant cancer cells) in other organs and systems.
Anatomy of the uterus: photo and wall structure
The organ is three-layered. It consists of: perimeter, myometrium and endometrium. The surface of the uterine wall is covered by the serous membrane of the peritoneum - the initial layer. At the next – middle level – the tissues thicken and have a more complex structure. Plexus of smooth muscle fibers and elastic connective structures form bundles that divide the myometrium into three internal layers: internal and external oblique, circular. The latter is also called the average circular. It received this name in connection with the structure. The most obvious is that it is the middle layer of the myometrium. The term “circular” is justified by a rich system of lymphatic and blood vessels, the number of which increases significantly as it approaches the cervix.
Bypassing the submucosa, the uterine wall after the myometrium passes into the endometrium - the mucous membrane. This is the inner layer, reaching a thickness of 3 mm. It has a longitudinal fold in the anterior and posterior region of the cervical canal, from which small palm-shaped branches extend at an acute angle to the right and left. The rest of the endometrium is smooth. The presence of folds protects the uterine cavity from the penetration of vaginal contents that are unfavorable for the internal organ. The endometrium of the uterus is prismatic; on its surface there are uterine tubular glands with glassy mucus. The alkaline reaction they provide preserves the viability of sperm. During ovulation, secretion increases and substances enter the cervical canal.
Erosion
So, what “reactive changes in the epithelium” means is clear. Now we should delve into the study of this topic and consider specific diseases.
Cervical erosion is a defect consisting of damage to the notorious squamous epithelium around the external os.
Of course, the cause is the inflammatory process. Erosion occurs in most women who have had cervicitis and endocervicitis. Although there is still a version according to which the cause is a change in the level of steroid sex hormones. There is some truth in this, since clinical observations have helped identify symptoms of erosion during pregnancy. In the postpartum period, they disappear as the hormonal levels stabilize.
Erosion is characterized by a recurrent, long-term, persistent course. This disease cannot be treated with conservative therapy. But unfortunately, diagnosis is difficult, since women have no characteristic complaints. In addition, this disease, which is caused by reactive changes in epithelial cells, is also asymptomatic.
Pathology can be detected during a visual examination of the cervix, as well as through colposcopy.
Uterine ligaments: anatomy, purpose
In the normal state of the female body, the uterus, ovaries and other adjacent organs are supported by the ligamentous apparatus, which is formed by smooth muscle structures.
The functioning of the internal reproductive organs largely depends on the condition of the muscles and fascia of the pelvic floor. The ligamentous apparatus consists of suspension, fixation and support. The combination of the properties of each of them ensures the normal physiological position of the uterus among other organs and the necessary mobility. Composition of the ligamentous apparatus of the internal reproductive organs
| Apparatus | Functions performed | Ligaments forming the apparatus |
| Suspensory | Connects the uterus to the walls of the pelvis | Paired wide uterine |
| Supporting ligaments of the ovary | ||
| Own ligaments of the ovary | ||
| Round ligaments of the uterus | ||
| Fixing | Fixes the position of the organ and stretches during pregnancy, providing the necessary mobility | Main ligament of the uterus |
| Vesicouterine ligaments | ||
| Sacrouterine ligaments | ||
| Supportive | Forms the pelvic floor, which is a support for the internal organs of the genitourinary system | Muscles and fascia of the perineum (outer, middle, inner layer) |
The anatomy of the uterus and appendages, as well as other organs of the female reproductive system, consists of developed muscle tissue and fascia, which play a significant role in the normal functioning of the entire reproductive system.
Female body
Representatives of the fair sex differ in many ways from men. In addition to external signs, there are also internal structural features of the body. Thus, representatives of the weak half of humanity are able to reproduce their own kind and feed them. A woman’s uterus, ovaries, pituitary gland and other organs play a major role in this process. Men are structured more primitively and simply.
Characteristics of the hanging apparatus
The suspensory apparatus consists of paired ligaments of the uterus, thanks to which it is “attached” at a certain distance to the walls of the pelvis. The broad uterine ligament is a transverse fold of the peritoneum. It covers the body of the uterus and the fallopian tubes on both sides. For the latter, the structure of the ligament is an integral part of the serous covering and mesentery. At the lateral walls of the pelvis it passes into the parietal peritoneum. The suspensory ligament arises from each ovary and has a wide shape. Characterized by durability. The uterine artery runs inside it.
The own ligaments of each of the ovaries originate from the uterine fundus on the posterior side below the branch of the fallopian tubes and reach the ovaries. The uterine arteries and veins pass inside them, so the structures are quite dense and durable.
One of the longest suspensory elements is the round ligament of the uterus. Its anatomy is as follows: the ligament looks like a cord up to 12 cm long. It originates in one of the corners of the uterus and passes under the anterior sheet of the broad ligament to the internal opening of the groin. After which the ligaments branch into numerous structures in the tissue of the pubis and labia majora, forming a spindle. It is thanks to the round ligaments of the uterus that it has a physiological inclination anteriorly.
Erythroplakia
When studying conditions in which squamous epithelial cells with reactive changes are observed, it is necessary to talk about this disease. Erythroplakia is a precancerous pathological condition in which the exocervix mucosa atrophies.
It is also asymptomatic. Sometimes mucous discharge and bleeding are observed. The causes are the same as in previous cases, but there may still be a burdened heredity. Scientists have not yet been able to prove the existence of a connection between erythroplakia and chromosomal and gene aberrations. However, according to statistics, the likelihood of developing the disease is much higher in those girls in whose family it has already occurred among women.
By the way, another cause of inflammation with reactive changes in the epithelium can be trauma. Cervical rupture often occurs during childbirth, hysteroscopy, abortion and curettage.
With erythroplakia, all natural processes of renewal, as well as maturation and further rejection of exocervix cells are disrupted. This leads to an imbalance between the cells of several layers of the membrane at once. Over time, the vaginal mucosa becomes very thin.
The disease is asymptomatic, only severe, advanced cases are accompanied by bleeding.
If squamous epithelial cells with reactive changes are found, and it turns out that this has led to erythroplakia, surgical treatment is prescribed. Conservative therapy is pointless. Either minimally invasive intervention or conization of the cervix is indicated.
Structure and location of fixing ligaments
The anatomy of the uterus should have suggested its natural purpose - bearing and giving birth to offspring. This process is inevitably accompanied by active contraction, growth and movement of the reproductive organ. In this connection, it is necessary not only to fix the correct position of the uterus in the abdominal cavity, but also to provide it with the necessary mobility. Fixing structures arose precisely for such purposes.
The main ligament of the uterus consists of plexuses of smooth muscle fibers and connective tissue, radially located to each other. The plexus surrounds the cervix in the area of the internal os. The ligament gradually passes into the pelvic fascia, thereby fixing the organ to the position of the pelvic floor. The vesicouterine and pubic ligamentous structures originate at the lower anterior part of the uterus and attach to the bladder and pubis, respectively.
The uterosacral ligament is formed by fibrous fibers and smooth muscles. It extends from the back of the cervix, envelops the rectum on the sides and connects to the fascia of the pelvis on the sacrum. In a standing position, they have a vertical direction and support the cervix.
What happens to the female body after surgery?
After removal of the uterus, a woman changes not only internally, but also externally. Most representatives of the fair sex note an internal emptiness in moral and physical terms. If a woman is of childbearing age, then in addition to depression, she feels helpless and useless.
After hysterectomy, many women are recommended hormone replacement therapy. This treatment allows you to maintain internal ligaments and muscles in tone.
Supporting apparatus: muscles and fascia
The anatomy of the uterus implies the concept of “pelvic floor”.
This is a set of muscles and fascia of the perineum that make it up and perform a function that supports the woman’s internal genital organs. The pelvic floor consists of an outer, middle and inner layer. The composition and characteristics of the elements included in each of them are shown in the table: Anatomy of the female uterus - structure of the pelvic floor
| Layer | Muscles | Characteristic |
| Outer | Ischiocavernosus | Steam room, located from the ischial tuberosities to the clitoris |
| Bulbous-spongy | The steam room wraps around the entrance to the vagina, thereby allowing it to contract | |
| Outdoor | Compresses the anus with a “ring”, surrounds the entire lower rectum | |
| Superficial transverse | Poorly developed paired muscle. Originates from the ischial tuberosity on the inner surface and attaches to the perineal tendon, connecting with the muscle of the same name coming from the reverse side | |
| Middle (genitourinary diaphragm) | m. sphincter urethrae externum | Compresses the urethra |
| Deep transverse | The steam room is located between the symphysis, pubis and ischium. | |
| Internal (pelvic diaphragm) | Pubococcygeal | Paired branches m. levator ani, which raises the anus. Well developed. |
| Iliococcygeal | ||
| Ischiococcygeal |
The normal anatomy of the uterus and appendages is ensured precisely by the pelvic floor, which is the main support of the internal organs of the genitourinary system. The correct location of organs is the key to their healthy functioning. Damage and significant weakening of the pelvic floor muscles threatens prolapse and even loss of organs.
Pathologies and anomalies
As a result of various adverse effects, the structure of the uterus or its position in the pelvic cavity may be disrupted.
Among the anomalies of the structure of the uterus, the following forms are distinguished:
- Organ doubling .
At the same time, there is always a doubling of the vagina. Most often, one of the uteruses is better developed than the other. In this case, a normal monthly cycle occurs in both uteruses, and pregnancy can develop in each of them. - Bicornuate uterus .
With this anomaly in the fundus, the organ is divided into two horns that connect at the cervix. Clinically, this deviation is manifested by menstrual irregularities, miscarriages and infertility. One of the horns may be underdeveloped (in this case, it looks like a cord or cavity formation communicating with the uterus). - Saddle-shaped (arched) uterus .
It is a variant of a bicornuate uterus, in which the separation of the fundus is minimally expressed. Most often, this anomaly is asymptomatic and is an incidental finding. - Intrauterine septum .
This is a malformation of the organ in which the uterus is divided into two cavities, which are either completely isolated from each other (complete septum) or communicate with each other in the cervical area (incomplete septum). Clinically, a uterine septum is manifested by habitual miscarriages, and less commonly by the inability to become pregnant.
The most common forms of abnormal location of the uterus are the following:
- Uterine prolapse .
In this case, the vaginal part of the cervix will not stand beyond the border of the genital slit. Otherwise, they talk about uterine prolapse. - Elevation of the uterus .
In this case, the fundus of the uterus is located above the upper plane of the pelvis. Elevation of the organ can be due to adhesions, accumulation of menstrual blood with atresia of the hymen, or with tumors of the rectum. - Rotation of the uterus. With this anomaly, the cervix and body of the uterus rotate in one direction. Unlike rotation, when the uterus is twisted, the cervix remains in place, and only the body turns.
- Displacement of the entire uterus .
This anomaly can manifest itself in various forms: displacement forward (anteposition), backward (retroposition), left or right (synistroposition or dextroposition).
Diseases
Pathological neoplasms are the first type of uterine diseases.
Uterine fibroids.
This is a benign tumor originating from the muscle layer. There are several types of myomatous nodes:
- Submucosal. Occurs most often in women of fertile age;
- Intramural nodes are located deep in the myometrium;
- Subserous nodes are localized outside the uterus, adjacent to the perimeter.
The main symptoms of uterine fibroids are heavy menstruation, miscarriages, and infertility.
Uterine fibroids.
If uterine fibroids contain mainly myocytes in their structure, then fibroma is a benign tumor consisting of connective tissue cells. The same forms of fibroma are distinguished as in the classification of fibroids. Separately, uterine fibroids are distinguished - a tumor containing muscle cells, but with the obligatory inclusion of fibrous tissue. The clinical manifestations of fibroids are identical to those of uterine fibroids.
Endometrial polyps are benign growths of blood vessels covered with epithelium. There are several types of polyps:
- fibrous - pale, round or oval, dense, smooth formations on a stalk, up to 15 mm in size;
- glandular-cystic - large (up to 60 mm), oblong, smooth, pale pink, gray-pink or yellowish;
- adenomatous - dull gray formations up to 15 mm in size.
Polyps may be asymptomatic or cause bleeding, pain and infertility.
Prolapse of the reproductive organ
Prolapse (loss) of the female reproductive organs is the movement of the vagina, cervix or uterine body beyond the genital opening.
There are three degrees of genital prolapse:
- I degree (not true prolapse): the cervix prolapses, but it does not extend beyond the entrance to the vagina;
- II degree: incomplete prolapse - movement of the cervix beyond the border of the genital fissure, but the uterus is in the pelvic cavity;
- III degree: complete prolapse - the entire uterus falls out.
The main cause of uterine prolapse is dysfunction of the ligamentous apparatus. This can be caused by connective tissue dysplasia, inflammatory and adhesive processes in the pelvis, impaired innervation and blood supply to the genital organs.
At the first stage of prolapse, there may be no complaints. Sometimes women note a feeling of heaviness in the perineum, discomfort when walking, pain in the lower back and sacrum.
The most characteristic symptom of the second and third stages is a formation that has fallen outside the genital slit.
Upon examination, the prolapsed parts of the cervix and body of the uterus have a bluish tint. The reason for this is poor circulation in the prolapsed areas of the organ.
Conservative management of prolapse of the female reproductive organs is impossible! The only way to treat this pathology is surgery.
The operation is aimed at returning organs to their physiological location, restoring and strengthening the supporting structures of the uterus and treating associated pathologies.
"Uterine rabies"
This term hides two diseases that belong more to the field of pathological psychology than gynecology.
Nymphomania (“disease of forest nymphs”) is female hypersexuality, excessive attraction to a man. This disorder is manifested by constant sexual dissatisfaction and the desire to constantly change sexual partners.
Hysteria (“the monkey of all diseases”) is a disorder characterized by a pathological need to attract attention to oneself. Although this condition also occurs in men, it is most pronounced in women. Hysteria can manifest itself with almost any known symptoms - uncontrollable laughter and/or crying, convulsive seizures, fainting, blindness, deafness, muteness, loss of sensitivity. It is not difficult to distinguish hysteria from a true disorder. It is enough to remember that hysteria manifests itself only in the presence of people whose attention the patient is trying to achieve.
Both nymphomania and hysteria require treatment from a psychiatrist and psychotherapist. But sometimes these disorders reach such severity that they require differential diagnosis with diseases of the nervous system (epilepsy, damage to the frontal lobes of the brain, stroke).
"Dense uterus"
A dense uterus is not an independent disease, but a symptom that accompanies the development of many pathological conditions. Uterine thickening means focal or total thickening of its walls, identified during a gynecological examination. The most common causes of the development of a dense uterus are myomatous nodes and foci of adenomyosis.
Adenomyosis (internal endometriosis) is a benign disease, which is based on the growth of the endometrium into the muscular layer of the uterus. The main symptoms to suspect adenomyosis are menstrual irregularities, intense dull pain in the lower abdomen, pain during sexual intercourse, and “chocolate”-colored discharge in the middle of the cycle.
If during the examination the gynecologist reveals a hardening of the uterus, an ultrasound should be performed to identify the cause.
The structure of the ovaries and appendages
The anatomy of the uterus and ovaries are reproductive organs connected to each other through the fallopian tubes. The ovaries are the sex glands located on either side of the uterus. Inside them, during the menstrual cycle, eggs mature, which then enter the uterine cavity through the fallopian tubes.
The ovaries are supported by the suspensory ligament and mesentery. Unlike the uterus, they are not covered with peritoneum. The structure of the ovary is based on the medulla and cortex. The latter contains mature follicles. On the inside, a granular layer is adjacent to the wall, in which the egg lies. It is surrounded by a radiant crown and a transparent zone.
During ovulation, the follicle approaches the outer layer of the ovary and bursts. This releases the egg and enters the uterine cavity through the fallopian tube. The burst follicle replaces the corpus luteum, which gradually disappears in the absence of pregnancy. If fertilization occurs, the corpus luteum continues to exist throughout the entire period to perform intrasecretory functions.
The surface of the ovaries is covered with a white membrane formed by connective tissue. Each ovary is surrounded by appendages, which have a convoluted shape and consist of longitudinal and transverse tributaries. They are considered to be vestigial formations.
Classification
After cytological analysis, the following reactive changes in the squamous epithelium are revealed:
- Exudative. The woman is found to have destroyed neutrophilic leukocytes. The smear contains fragments of cells and nuclei. The preserved, intact ones are in a state of phagocytosis.
- Reparative. The name for this type of change was given by the repair and subsequent epithelization occurring in the defective surface of the layers. Based on the results of the analysis, cells of increased size are detected. It is because of them that tissue grows, which replenishes the affected areas. The nuclei become larger, but do not lose their clear contours. No chromatin accumulation is observed. By the way, it has a soft-grained structure.
- Degenerative. Manifested by shrinkage of the cell nucleus. Disturbances in the structure of the nuclear membrane and chromatin are also observed. Proliferation of the epithelium indicates a chronic inflammatory process.
When talking about reactive changes in the squamous epithelium, it is necessary to note that cytological analysis also often reveals a combination of inflammatory changes. Often reparative ones are combined with degenerative and proliferative ones.
In such cases, multinucleate cells with large nuclei are detected. The cytological picture strongly resembles dysplasia or cancerous conditions. If we talk about inflammatory atypia, it is characterized by a uniform distribution of chromatin. The lumps have unclear contours.
The fallopian tubes
A paired organ through which an egg from the abdominal cavity enters the uterus. The fallopian tubes are oval-shaped ducts that run at the top of the broad ligament of the uterus. Their length can be up to 13 centimeters, and their diameter is 3 mm. Transportation of the egg is carried out using the uterine and abdominal openings, the name of which corresponds to the cavities into which it exits.
The fallopian tubes consist of:
- uterine part - located in the thickness of the uterus;
- isthmus - the narrowest part with thick walls;
- ampoules;
- funnels - through their lumen the egg enters the fallopian tube;
- fimbria - they direct the egg to the funnel.
The inside of the tube is lined with a mucous membrane with ciliated epithelium and longitudinal folds, the number of which increases as it approaches the abdominal opening. On the outside, the fallopian tubes are covered with a serous membrane.
Pathogenesis
Reactive changes in the epithelium occur due to a woman contracting an infection. This usually happens due to unprotected sexual intercourse with an untested partner.
About 50% of all infections are bacterial in origin. Inflammation of the vaginal membranes provokes a similar process occurring in the cervix.
Interestingly, in some cases even bacteria that make up the natural microflora of the genital tract are infectious agents. But this only happens if the immune system is weakened.
An initial examination aimed at identifying reactive changes in the epithelium reveals inflammation. Cytology analysis shows the content of a large number of leukocytes with destroyed nuclei, eosinophilic and lymphoid elements. If we talk about microflora, then with reactive changes in the epithelium it becomes mixed.
If inflammation is detected in time, it can be safely overcome with the help of adequate antibacterial treatment. The therapy is completed by restoring the microflora - for this, prebiotics are used.
Structure of the circulatory system
The blood supply to the reproductive organ occurs thanks to the uterine artery, which is a branch of the internal iliac artery. The anatomy of the uterus and fallopian tubes involves the outflow of blood from two sides, so the artery has two branches. Each of them is located along the broad ligament, then dividing into smaller vessels going to the anterior and posterior surfaces of the organ. Near the uterine fundus, the vessel branches again to provide blood flow to the fallopian tubes and ovaries.
The uterine veins are formed from the venous plexus, into which venous blood drains. From here the veins originate, which then flow into the internal iliac, ovarian veins and the plexuses of the rectum. Venous drainage after the uterine and ovarian veins passes to the iliac and inferior vena cava.
Diseases of the female organ
Many representatives of the fairer sex have to deal with pathologies that affect the reproductive system. These include endometritis, fibroids, uterine prolapse in women and other diseases. Some of them can be safely treated and have a favorable prognosis. Others lead to such a horrifying conclusion as hysterectomy. Women who have had to undergo this procedure feel depressed and inferior. Let's look at a few examples of pathologies of the female organ.
Innervation of the uterus and other female reproductive organs
The internal genital organs are innervated by the sympathetic and parasympathetic autonomic nervous system. The nerves going to the uterus are usually sympathetic. On their way, spinal fibers and structures of the sacral nerve plexus are attached. Contractions of the uterine body are regulated by the nerves of the superior hypogastric plexus. The uterus itself is innervated by branches of the uterovaginal plexus. The cervix usually receives impulses from the parasympathetic nerves. The ovaries, fallopian tubes, and adnexa are innervated by both the uterovaginal and ovarian plexuses of nerves.
Layers
The structure of the uterine wall includes 3 layers:
- serous membrane (perimetry) - represents the peritoneum;
- internal mucous tissue - endometrium;
- muscular layer - myometrium.
There is also a parametrium - a layer of pelvic tissue, which is located at the level of the cervix at the base of the broad ligaments of the uterus, between the layers of the peritoneum. The location between the organs provides the necessary mobility.
to contents ^
Endometrium
The structure of the layer is shown in the figure.
The mucous epithelium is rich in glands, characterized by good blood supply, and is sensitive to damage and inflammatory processes.
The endometrium has 2 layers: basal and functional. The thickness of the inner shell reaches 3 millimeters.
to contents ^
Myometrium
The muscular layer is composed of intertwined smooth muscle cells. Contractions of myometrial sections on different days of the cycle are regulated by the autonomic nervous system.
to contents ^
Perimetry
The serous outer membrane is located on the anterior wall of the uterine body, completely covering it.
At the border with the cervix, the layer bends and is transferred to the bladder, forming the vesicouterine space. In addition to the posterior surface of the body, the peritoneum covers a small area of the posterior vaginal vault and the rectum, forming a rectal-uterine pouch.
These depressions and the location of the uterus in relation to the peritoneum are marked in the figure depicting the topography of the female genital organs.
to contents ^
Functional changes during the monthly cycle
The uterine wall is subject to changes both during pregnancy and throughout the menstrual cycle. The sexual cycle in the female body is characterized by a combination of processes occurring in the ovaries and the mucous membrane of the uterus under the influence of hormones. It is divided into 3 stages: menstrual, postmenstrual and premenstrual.
Desquamation (menstrual phase) occurs if fertilization does not occur during the ovulation period. The uterus, a structure whose anatomy consists of several layers, begins to reject the mucous membrane. The dead egg also comes out with it.
After the functional layer is rejected, the uterus is covered only with a thin basal mucosa. Postmenstrual recovery begins. The ovary re-produces the corpus luteum and a period of active secretory activity of the ovaries begins. The mucous membrane thickens again, the uterus prepares to receive a fertilized egg.
The cycle continues continuously until fertilization occurs. When the embryo implants into the uterine cavity, pregnancy begins. Every week it increases in size, reaching 20 or more centimeters in length. The birth process is accompanied by active contractions of the uterus, which contributes to the oppression of the fetus from the cavity and its return to prenatal size.
The uterus, ovaries, fallopian tubes and appendages together form a complex system of female reproductive organs. Thanks to the pelvic floor and mesentery, the organs are securely fixed in the abdominal cavity and are protected from excessive displacement and prolapse. The blood flow is provided by a large uterine artery, and the organ is innervated by several nerve bundles.
Cervical treatment methods
Therapeutic measures for diseases of the cervix are aimed at eliminating the affected area and preventing the growth of this area into healthy areas of the organ.
There are several approaches to treating the cervix:
- conservative;
- surgical;
- physiotherapeutic.
The most effective method is the surgical method, taking into account a number of features. Surgical interventions are carried out in the first two weeks of the monthly cycle, when the level of estrogen is elevated, and the body's regenerative abilities contribute to the speedy healing of postoperative wounds.
Coagulation
Coagulation is a minimally invasive intervention, the purpose of which is to stop bleeding using clotted blood and “cauterization” of the pathological area on the vaginal surface of the cervix. This technique is effective for diseases such as polyps, endometriosis of the cervical canal, leukoplakia.
Benefits of coagulation:
- rapid tissue regeneration;
- additional antiseptic;
- small area of exposure, without affecting healthy tissue;
- no complications (bleeding).
Diathermocoagulation
The cervix (photo of diathermocoagulation is given below) with pseudo-erosions is an indication for diathermocoagulation. Treatment involves applying high-frequency electric current to the affected area, creating a high temperature and causing tissue proteins to coagulate. The goal of treatment is to prevent possible complications.
Contraindications for such manipulation will be:
- pregnancy;
- malignant neoplasm of the cervix;
- second half of the monthly cycle.
Laser treatment
Laser coagulation (vaporization) is an electrosurgical method for treating cervical erosions of various sizes, and less commonly, polyps and endometriosis. The essence of the procedure is the impact of a laser beam on the affected tissue, where mechanical energy is converted into thermal energy. Coagulation of tissue occurs where the beam was exposed.
Advantages of the technique:
- painlessness;
- ease of use;
- minimal risk of complications;
- the possibility of using the method for nulliparous patients.
The disadvantage is the high cost.
Cryodestruction
Cryodestruction (cryotherapy, cryoablation) – exposure of the lesion to very low temperatures (up to 200°), using a cryodestructor. Cooling of the tissue occurs under the influence of liquefied gas (nitrous oxide, liquid nitrogen, carbon dioxide) emanating from the cylinder and sharply changing the temperature when transitioning to a gaseous state. At the point of contact, the blood supply is cut off and the tissue dies.
Indications for use:
- ectropion (no more than 3 cm);
- pseudo-erosion;
- leukoplakia;
- erythroplakia.
Cryodestruction should not be used if the following is present on the cervix:
- large lesions (more than 3 cm);
- malignant neoplasms;
- postoperative scars or stitches;
- inflammatory diseases.
Radio wave therapy
Treatment with radio waves is one of the methods for cauterizing large erosions or pseudo-erosions on the cervix. The essence of the method is the impact of high-frequency waves emanating from the tip of the device on the focal area and the subsequent evaporation of these tissues.
A radio wave knife, used during the action of high-frequency waves, excises tissue, disinfects and coagulates damaged vessels. The rehabilitation period passes quite quickly. Contraindications are the same as for other types of coagulation.
Conization
Conization is a surgical intervention, the purpose of which is to remove part of the cervix and cervical canal where a cancerous tumor or precancerous disease is located and to prevent the progression of the identified pathology.
The decision on the need to perform such a procedure is based on the following data:
- cervical biopsy (presence of atypical cells);
- examination of the cervix in the mirrors and detection of dysplasia (deformation) of 3-4 degrees;
- medical history and life history (precancerous conditions were previously identified - erosion, proliferative leukoplakia or cervical polyps);
- patient complaints.
In advanced conditions there is an unfavorable outcome. Surgery does not guarantee complete resolution of the disease, but it is quite possible to stop the progression.
Primiparous patients should remember that after conization, complications during pregnancy are possible. This is due to the inability of the cervix to hold the fetus until it is fully mature, and there is an increased risk of premature labor.
Amputation
Cervical amputation is a surgical procedure aimed at removing the lower segment of the uterus in order to prevent further progression of the cancerous tumor.
In addition to cancer, indications for surgery will be:
- precancerous conditions (leukoplakia, multiple or single polyps, extensive erosion of the cervix);
- ectropion (more than 3 cm);
- postoperative or post-traumatic defects of the cervix;
- foci of endometriosis;
- congenital pathologies of the cervix - lengthening, narrowing or obstruction.
A common complication in the postoperative period is stenosis (impaired patency) of the cervical canal, as well as bleeding due to failure of the sutures. Cervical pathology is a pressing problem in the modern world.
This is due to a number of reasons: blurred clinical picture, errors by medical personnel during diagnosis and treatment, patients’ failure to comply with simple rules of personal hygiene, an increase in the number of cases of genetic predisposition, and frequent changes of sexual partners.
The information and photographs given above describe only part of the entire pathology encountered. Due to the large number of cervical diseases and the presence of provoking factors, women should consult a gynecologist several times a year.
Eliminating Risk Factors
Treatment of cervical leukoplakia, regardless of its form and complexity, must be treated in a complex manner. Therapy should begin with eliminating the factors that were the root cause for the development of the pathological process and accompanying malfunctions in the body.
It is also worth making sure that the patient does not have infections and inflammatory diseases, somatic and endocrine disorders. It is equally important to stop smoking, and, as an option, to free the oral cavity from metal dentures.
Treatment tactics
In cases where the doctor discovers problems with the cervix, he should tell you what needs to be done next. So, first of all, the specialist will perform a colposcopy, take material for cytological examination and, if necessary, offer a biopsy. A complete examination allows you to determine what causes cervical erosion. It is also important to do microflora smears to determine if there are any infectious diseases. It is mandatory to find out whether the patient has HIV, syphilis or viral hepatitis. In addition, the gynecologist can give a referral for examination for the presence of trichomonas, ureaplasma, HPV, chlamydia, mycoplasma, and gardnerella.
Prevention
Every girl is recommended to undergo examination by a gynecologist at least once a year. Based on all of the above, it could be understood that many serious illnesses can be asymptomatic, and when they make themselves felt, it will be too late for conservative therapy.
Treatment is also always prescribed on an individual basis. The origin of the inflammation, the patient’s age, whether she is planning a pregnancy and, of course, the type of pathology are taken into account.
But the most important thing is a responsible approach to choosing sexual partners. There may not be a permanent man, but it is always necessary to defend yourself. Because it is STDs that lead to reactive changes.
And you also need to constantly maintain your immunity and strengthen it regularly. Because weakened body defenses provide the best conditions for the development of the virus.
And of course, it is necessary to select oral contraceptives with caution. The doctor selects them. Choosing the wrong pills can have serious consequences. And disrupted hormonal levels are one of the causes of reactive changes.
Signs
Some symptoms will help identify reactive changes. Firstly, redness appears on the mucous membrane, causing discomfort.
Secondly, cytological analysis will help identify deviations from the norm in the composition of the smear - the number of leukocytes is usually increased, and epithelial cells may have structural changes.
A woman may notice the appearance of an unpleasant smell of discharge and an increase in its volume. The pathological condition is indicated by bloody discharge not associated with menstruation.
Papillomavirus
Most often, people do not even suspect that they have HPV in their bodies. For some, the disease occurs in a latent form. This means that people are carriers of the virus, but they do not have any manifestations. In the subclinical form, cytological changes are diagnosed. Clinically expressed HPV is determined when exophytic and endophytic condylomas are visible.
The most common are the 16th and 18th serotypes of papillomavirus. Infection, as a rule, goes completely unnoticed and is not accompanied by the appearance of any symptoms. But at the same time, the virus infects cells, it is integrated into their genetic code, and the replication of infected elements begins. This ultimately leads to their degeneration and causes the appearance of dysplasia or cancer.
But it is believed that the individual susceptibility of the epithelium and congenital defects in defense mechanisms play an important role in the development of diseases.
Alternative medicine
Some are starting to look for alternative methods. The most popular are douching with a diluted infusion of calendula (1 tsp in ¼ glass of water), eucalyptus (1 tsp diluted in a glass of water), tampons with sea buckthorn oil or mummy.
But these are not all the options for how the cervix can be treated with folk remedies. Some healers recommend brewing St. John's wort for douching at the rate of 1 tbsp. l. for a half-liter jar of boiling water. The herb must be boiled for about 10 minutes and infused for at least half an hour.
If you decide to refuse qualified help and are treated with the indicated methods, then regularly visit a gynecologist in order to monitor the condition of the cervix. This is the only way to see the deterioration in time and try to correct the situation.
New therapeutic techniques
Relatively new treatment methods are organotherapy, mistletoe therapy, and photodynamic therapy.
Organotherapy uses organopreparations based on intracellular biologically active substances from glands and organs of animal and plant origin.
Mistletoe therapy involves the use of medicines from mistletoe, which activates the body's protective immune system. This suppresses tumor growth and the possibility of metastasis.
Photodynamic therapy involves the use of photoactive substances that are introduced into the body and then exposed to a laser. This is effective in the treatment of not only inflammatory pathologies, but also malignant tumors.
Modern hardware technologies
Surgical treatment consists of eliminating the area of dysplasia.
- Cauterization. This technique is recommended if there is no effect from conservative therapy. Used for grades 2 and 3. In this case, electrocoagulation and cryodestruction are used. The latter is more gentle, but there remains a risk that some atypical cells will not be frozen sufficiently and will remain alive.
- Laser coagulation. This cauterization method is quite effective and painless. Complications after it are practically excluded
- Radio wave destruction. With this method, the affected areas are cauterized using radio waves of a special frequency. This technique is one of the more promising. Its advantages are that the surrounding tissues are little involved. Healing occurs within a month.
The big advantage is that the muscle cells of the cervix are not affected. There is no scar left after the procedure. And this guarantees the absence of complications during childbirth.
- Electroconization. This method is used for severe cases. With its help, pathologically altered cells are eliminated throughout the entire thickness of the epithelium.
- Conization is the elimination of a cone-shaped section of the cervix. It is used when previous methods are ineffective.
Therapy using chemical methods is carried out with special drugs that have a cauterizing effect. After such exposure, a crust forms, which after a few days comes off on its own. This is used only for small affected areas. The procedure may need to be repeated several times.
Diagnostics of background processes
On examination, pseudo-erosion looks like a red spot of irregular shape. It stands out against the background of pale mucous membrane. When performing a colposcopy, it becomes clear that the problem areas are covered with red papillae of a round or oblong shape, because of which the surface looks like velvet. You shouldn’t be afraid of colposcopy, it’s just an examination using a special device that can enlarge the area 30-40 times.
Diagnosis of a disease such as leukoplakia is also not difficult. In some patients, the keratinized layers of cells are visible to the naked eye; they appear as white plaques that rise on the ectocervix (the part of the cervix that protrudes into the vagina). In others, they can only be detected during colposcopy. To clarify the diagnosis, cervical tissue can be treated with iodine solution. The affected keratinized areas do not turn brown; they look like a surface covered with a whitish film. To determine the nature of leukoplakia (simple or with atypical cells), a biopsy is necessary.
Also, during examination, the gynecologist may see cysts on the cervix. The reasons for their appearance are as follows:
- sexually transmitted infections that provoke the development of inflammatory diseases;
- injury to the cervix during childbirth, abortion, diagnostic curettage;
Cysts look like sacs filled with mucus. They arise from the nabothian glands, which appear as small white swellings. If there are malfunctions in their work, the ducts close. In the case when only one sac is visible upon examination, it is called an endometriotic cyst. But there are times when there are several of them. In such situations, the doctor says that these are Nabothian cysts on the cervix. It is advisable to find out the reasons for their occurrence. After all, their appearance can be caused by infections that need to be treated. As a rule, doctors recommend only one treatment method - removal of cysts. This is done by puncturing the sac, removing viscous mucus and treating the place where it appears.
Characteristics of background processes
Even in teenage girls, the gynecologist can see displacement of the columnar epithelium during examination. After colposcopy, it becomes clear that it is bright red in color. However, it is impossible to paint it with Lugol's solution. This condition is often called pseudoerosion or ectopia. It can be congenital or acquired. But these are not yet precancerous conditions of the cervix, so such erosions do not require treatment. You just need to monitor them regularly.
If the patient's mucous membrane of the cervical canal everts onto the vaginal part of the cervix, then this condition is called ectropion. This is a combination of scar deformation of cervical tissue and pseudo-erosion. Upon examination, the doctor may see a deformed neck with a slit-like or gaping pharynx with red areas of columnar epithelium. Often they can have a transformation zone.
Another background process is leukoplakia, the name of the disease is translated as “white spot”. With this disease, the stratified epithelium becomes locally keratinized. In this case, infiltrates form around the stromal vessels. Leukoplakia can be simple, then it is classified as a background process. If atypical cells appear with this disease, then we are talking about precancer.
Another disease is erythroplakia, but it is quite rare. This name literally translates as “red spot”. In this condition, the stratified epithelium atrophies and thins down to several layers. Intermediate cells disappear. Vessels are visible through the thinned epithelium, so the areas look like red spots.
Also, during examination, the doctor can see growths covered with epithelium. They are called polyps. These are bright pink formations that can be leaf-shaped or oblong. They hang from the throat of the cervix.
Cervicitis
In some cases, white spots appear in certain forms of cervicitis, an inflammatory process that affects the vaginal segment of the cervix. The disease is characterized by the following symptoms:
- dull or nagging pain in the lower abdomen;
- pathological discharge, mucous or mucopurulent consistency, which has an odor different from normal;
- pain during urination;
- discomfort during sexual intercourse.
Pathology is caused by sexually transmitted infections. They lead to the formation of erosion, which in some situations becomes an area of keratinization - a white spot.
To get rid of such white spots on the cervix, antibacterial or antiviral drugs are needed - the selection of drugs depends on the type of disease. If the cause of the pathology is an infection, not only the woman herself, but also her sexual partner undergoes therapy.
Degrees of dysplasia
In the diagnosis of dysplasia, the degrees are graded depending on the severity of changes in the epithelial layer.
- Easy. Cell structures are slightly changed. They are detected only in one third of the epithelium.
- Moderate. Characterized by a progressive change in intracellular structure. Changes are already detected in 2/3 of the epithelial layer.
- Severe (non-invasive cancer). Changes take place in all layers. But there is no germination into nearby tissues and vessels.
It is easier to prevent a disease than to treat it!
Nonspecific approaches to preventing cervical cancer are quite simple. To do this, you need to take measures to prevent infection with HPV and other STIs (using condoms). A later onset of sexual activity, a limited number of partners, and an orderly sex life can also have a certain positive effect. In addition, you should eliminate such bad habits as smoking, not have abortions, and avoid long-term use of oral contraceptives.
In cases of cervical tumors, the phrase “cancer vaccine” has ceased to be something fantastic, and the method has become available to a wide range of the population. Specific prevention of cervical cancer is the use of a vaccine against the human papillomavirus. Today, two drugs exist and are registered in most countries - Cervarix and Gardasil. Cervarix protects against the most oncogenic HPV serotypes 16 and 18, and Gardasil protects against four types of the virus (16, 18, 6, 11).
For the most effective prevention, it is recommended to administer vaccines to girls aged 10-14 years, before the onset of sexual activity and possible infection, however, vaccination of adult women, including those already infected, is also practiced. It has been proven that the administration of drugs in such cases helps to strengthen the body’s protective properties against HPV and speed up recovery even in the presence of precancerous changes.
On the Internet and other sources of information, you can find a lot of contradictory information pointing to the allegedly negative impact of vaccines against CC on a woman’s body; examples include a variety of terrible consequences, including death, but these conclusions are usually quite unfounded and not supported by reliable scientific evidence. data. Without vaccine prevention in general, humanity would still not have gotten rid of smallpox, children would have suffered from whooping cough and polio, millions of people would have died from infections that were preventable thanks to vaccinations. In this regard, you should not be afraid of HPV vaccines, because the risk of developing cancer is much more dangerous.
Since vaccination against cervical cancer is not included in the standard vaccination schedule for the population, it can be done at any antenatal clinic at the request of the woman or the girl’s parents for a fee.
Cervical cancer can be prevented even at the stage of development of precancerous changes (dysplasia), and if detected early, young women can often retain their ability to bear children.
All representatives of the fair sex must visit an obstetrician-gynecologist for a routine examination at least once a year, and if even the most seemingly insignificant symptoms occur, they should immediately consult a doctor.
Cervical cancer can and should be prevented by all available means, since successful prevention is the key to overall health and well-being.
Interpretation of colposcopy results
The results of colposcopy must be deciphered by the doctor after the examination. In order to correctly understand the interpretation of the data obtained, you should study the meaning of some terms and concepts:
- Stratified squamous epithelium, or MPE. This term refers to the normal epithelial cells that cover the vaginal portion of the cervix (exo- or ectocervix).
- Glandular (cylindrical) epithelium. This term refers to normal epithelial cells of the cervical canal, or endocervix.
Clinical manifestations and symptoms
Symptoms of cervical cancer are quite non-specific, at the initial stage of the disease they are quite scarce, so women often do not consult a doctor with such symptoms.
If the tumor is small, there may be discomfort in the pelvic area and discharge, including bloody discharge, from the genital tract. As the tumor progresses and its size increases, signs such as:
- Heavy bleeding (outside of menstruation, after menopause);
- Contact bleeding (during examination, digital examination, coitus);
- Pain in the pelvic area;
- Frequent, painful urination and defecation disorders;
- The appearance of urine and intestinal contents in the vaginal discharge (in advanced cases, when fistulas form in the bladder or rectum).
In addition to the described symptoms, there are also other general signs of malignant growth that are also found in cancer of other locations. Severe intoxication with metabolic products of the tumor, possible secondary changes in it in the form of necrosis, inflammation, as well as chronic blood loss can lead to prolonged fever, severe weakness, weight loss, and anemia.
If at least one of the described symptoms appears, you should immediately consult a doctor. Quite a large number of cancer cases are diagnosed at late stages due to the woman’s failure to visit a gynecologist on time or ignoring regular annual examinations.